
 Goizueta’s Diwas KC is committed to finding solutions for hospital operations that could translate into real improvements in terms of cost management. Here are some highlights from a 10-year career in healthcare research that could leave hospitals and health centers in considerably better shape.
Goizueta’s Diwas KC is committed to finding solutions for hospital operations that could translate into real improvements in terms of cost management. Here are some highlights from a 10-year career in healthcare research that could leave hospitals and health centers in considerably better shape.
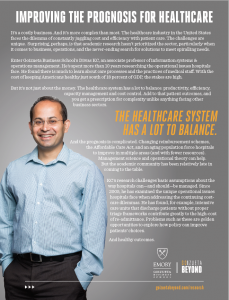
It’s a costly business. And it’s more complex than most. The healthcare industry in the United States faces the dilemma of constantly juggling cost and efficiency with patient care. The challenges are unique. Surprising, perhaps, is that academic research hasn’t prioritized the sector, particularly when it comes to business, operations, and the never-ending search for solutions to meet spiraling needs.
With the cost of keeping Americans healthy just south of 18 percent of GDP, the stakes are high.
But it’s not just about the money.
The healthcare system has a lot to balance: productivity, efficiency, capacity management and cost control. Add to that patient outcomes, and you get a prescription for complexity unlike anything facing other business sectors.
And the prognosis is complicated. Changing reimbursement schemes, the Affordable Care Act, and an aging population force hospitals to improve in multiple areas (and with fewer resources). Management science and operational theory can help. But the academic community has been relatively late in coming to the table.
While management science and behavioral theory could take up some of the slack in terms of exploring and framing solutions to needs and challenges, it’s only recently researchers have begun to look with acuity at how hospitals operate; and at what can be done to improve productivity, cost management and patient outcomes.
Diwas KC, Associate Professor of Information Systems & Operations Management, finds all of this a bit perplexing.
A pioneer in healthcare research, KC believes hospitals offer a particularly fertile environment for operations management research. His research challenges basic assumptions about the way hospitals can—and should—be managed. Since 2005, he has examined the unique operational issues hospitals face when addressing the continuing costcare dilemmas. He has found, for example, intensive care units that discharge patients without proper triage frameworks contribute greatly to the high-cost of re-admittance. Problems such as these are golden opportunities to explore how policy can improve patients’ choices.
The confluence of operational challenges balanced against the primary purpose of caregiving is such that the healthcare industry faces what KC describes as “some of the most pressing socioeconomic issues of our time – both in complexity and in scale.” A challenge, then, for academics to pursue research that has “real impact,” he says.
KC has spent the last 10 years exploring the unique operational issues hospitals face in addressing the on-going cost-care dilemma.
His work teases out the link between worker productivity and quality of care. And his findings, he says, have tended to be “surprising.”
Repurposing downtime
Spend a day in an average hospital and you’ll likely come away with the impression they are busy places: medical staff at maximum capacity and multitasking the norm.
In his paper Does Multi-Tasking Improve Performance? Evidence from the Emergency Department, KC challenges assumptions about the negative impact of multitasking on staff productivity. He finds that there is an optimal level – a kind of multitasking sweet spot – that can actually boost efficiency exponentially.
“Take the ER setting,” he says. “There is actually a considerable amount of downtime for doctors and nurses in this context, when they are waiting for lab work or X-rays for example. This is when they can perform routine tasks, or see other patients.”
Behavioral science sheds light on motivation and performance, says KC, meaning that there is an opportunity to reframe challenges and improve patient outcomes.
“Physicians typically falter when they feel bombarded with work,” he says. “But when things are presented as a ‘bit of a challenge’ they actually seem to thrive.”
Avoiding the bounce backs
Managing capacity is a major issue for hospitals – and nowhere more so in intensive care units. Cost is also a key factor.
KC’s research into capacity management in cardiac intensive care units, An Econometric Analysis of Patient Flows in the Cardiac ICU, reveals a critical link between how hospitals approach capacity and cost management and the potential for improved patient outcomes.
Current practice is such that a hospital will discharge a patient from the ICU to make room for intakes from the Operating Room – the principle criterion being capacity building. However when those patients are re-admitted, capacity remains an issue, costs increase and bottlenecking becomes a problem.
KC’s research finds that a triage approach to determine less severe conditions, combined with what he calls “step down” facilities offering less intensive care would significantly reduce the pressure on ICUs; reducing cost, improving patient care and mitigating the bounce back effect of readmission.
Improving choices
KC’s research also delves into the impact of policy and regulation on healthcare quality and patient care. As part of his on-going research, he has tracked the behavior of patients who had taken out health insurance in the wake of the Massachusetts Healthcare Act.
He has, so far, determined two effects of this kind of policy change.
The so-called “safety-net” hospitals that had provided care to uninsured patients prior to the reform have lost market share. But this is offset by an improvement in care for newly insured patients who are now able to pinpoint the hospital that best meets their short-, mid- and long-term needs.
“I want to research a field where the work you do can have real impact – to break down the noise and find real-world solutions to real-world problems,” he says. “In healthcare, there are multiple players and multiple decisions that aren’t made in isolation. So it’s difficult to make changes. But the magnitude of the problem and the need for quality and cost-effective care make this a field of study that is as compelling as it is vital for the health of the U.S.”










